According to the results of a phase III clinical trial, an experimental drug that interferes with cortisol receptors could, when combined with chemotherapy, become the new standard of care for patients with treatment-resistant ovarian cancer.
For the first time after years of research, a clinical trial shows an improvement in overall survival for platinum-resistant ovarian cancer. The phase III ROSELLA trial data, published today in The Lancet and presented at the prestigious American Society for Clinical Oncology (ASCO) conference, offers new hope.
The results demonstrate improved efficacy of chemotherapy when combined with an experimental molecule (called relacorilant) that blocks the pro-tumor effects of cortisol. This hormone, known for its role in the stress response, can make cancer cells more resistant to chemotherapy. The new treatment combination significantly improved both progression-free survival and overall survival, with the latter increasing by nearly 40%. Additionally, the safety profile was comparable to chemotherapy alone.
The clinical trial was conducted internationally, involving 117 centers across 14 countries. In Europe, it was coordinated by Domenica Lorusso – currently Head of Gynecologic Oncology at Humanitas San Pio X and Full Professor at Humanitas University – who was at the time Head of the Clinical Research Program at Gemelli Hospital in Rome.
“Ovarian cancer is one of the most aggressive and complex gynecologic cancers to treat,” says Prof. Domenica Lorusso. “Often diagnosed at advanced stages, it has a high mortality rate due to its tendency to develop resistance to standard drug therapies, particularly platinum-based drugs. That’s why the study results are so significant: they could lead to a change in treatment guidelines for this complex disease. This result was made possible thanks to collaboration between academia, industry, leading hospitals, and patient associations.”
The role of stress receptors
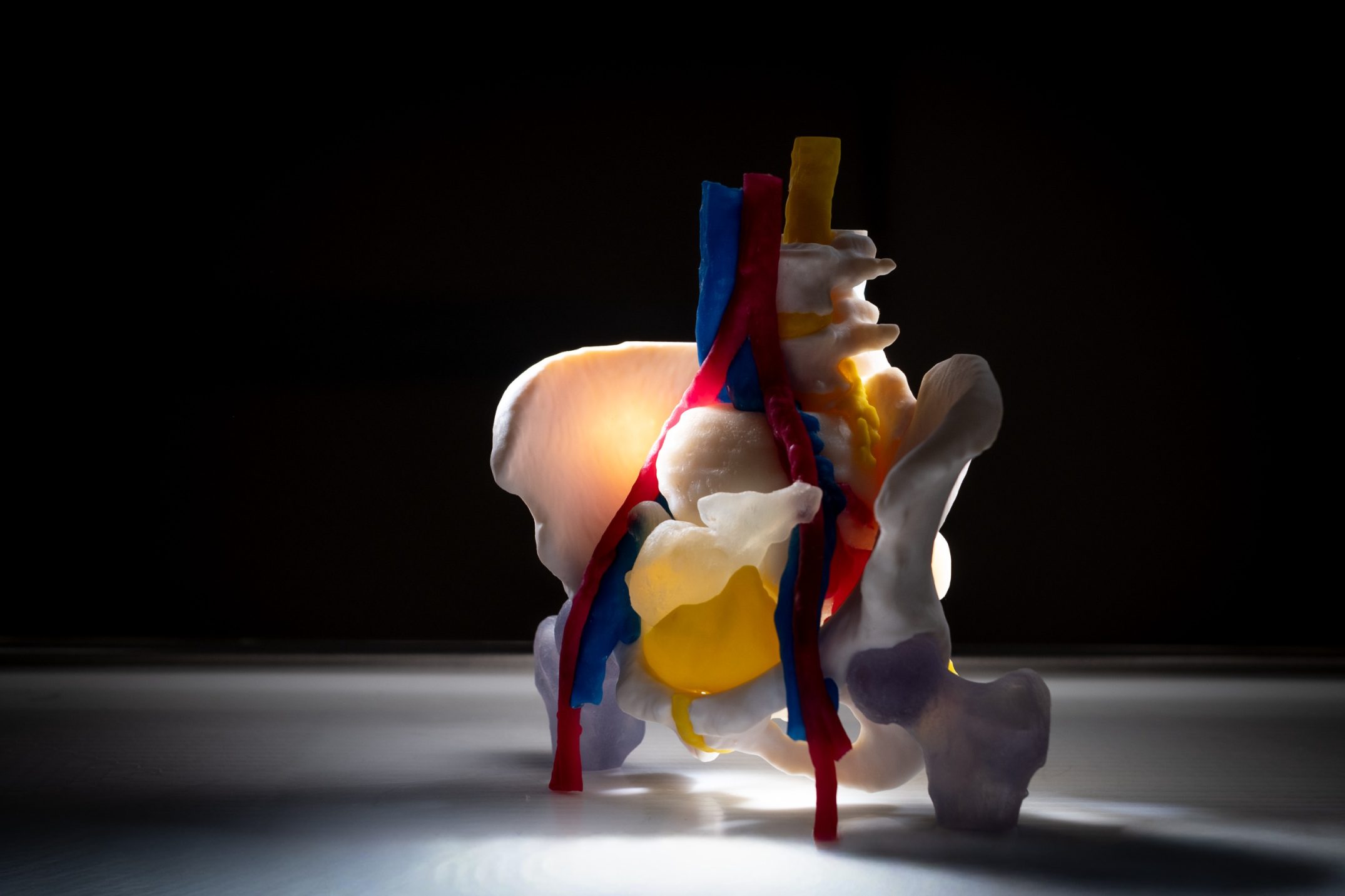
The experimental drug is designed to counter one of the main mechanisms of ovarian cancer resistance to chemotherapy: the overactivity of glucocorticoid receptors (GR).
Cortisol, known as the “stress hormone,” regulates many physiological processes, including stress and metabolism, but also plays a crucial role in cancer progression by stimulating glucocorticoid receptors on tumor cells. These receptors promote cell survival by reducing apoptosis (natural cell death) and increasing chemotherapy resistance. Unsurprisingly, high cortisol levels in ovarian cancer patients are associated with particularly poor prognosis.
The new molecule belongs to a class of compounds known as selective glucocorticoid receptor antagonists, which work by interfering with this mechanism, thereby making cancer cells more vulnerable to chemotherapy.
The clinical study
The study involved 381 women affected by this serious condition. Participants had already undergone multiple unsuccessful treatments, including bevacizumab, a commonly used drug that works by inhibiting the formation of blood vessels that feed the tumor.
Patients were divided into two groups: one group received a combination of relacorilant (a new selective glucocorticoid receptor antagonist) and nab-paclitaxel, a chemotherapeutic agent. The second group received only nab-paclitaxel.
The primary objective of the study was to determine whether adding relacorilant could slow disease progression and improve overall survival.
The results were very promising. Patients treated with the relacorilant and nab-paclitaxel combination showed a significant improvement in progression-free survival, reaching 6.5 months compared to 5.5 months for those receiving only nab-paclitaxel. Even more notable was the increase in overall survival: patients on the combination therapy reached a median survival of 16 months, compared to 11.5 months in the control group, a clinically significant improvement.
Another key finding was the good tolerability of the combined treatment: side effects were similar between the two groups, confirming the safety of this new therapeutic strategy.