Vaccination, early diagnosis, access to care and awareness are the tools to prevent hepatocellular carcinoma
World Hepatitis Day, celebrated each year on 28th July, was established by the World Health Organization (WHO) to mark the birthday of researcher Baruch Blumberg, Nobel Prize winner for identifying the hepatitis B virus (HBV) and developing the first vaccine. It is a crucial opportunity to shine a light on a group of silent but potentially serious diseases that affect millions of people around the world every year. Yet, with prevention, vaccination, screening, and treatment, many forms of hepatitis can be avoided, treated, and even cured. Getting vaccinated, maintaining a balanced diet, avoiding alcohol, and taking advantage of the free screenings offered by the National Health Service are simple yet essential actions to protect the liver and one’s overall health.
In Italy, it is estimated that around 250,000 people live with hepatitis B and about 300,000 with hepatitis C¹. These are significant numbers, but they have declined compared to ten years ago. The main reason for this shift is the major impact of direct-acting antiviral drugs for hepatitis C, which have cured over 250,000 people. Furthermore, in 1991, Italy was among the first countries to make hepatitis B vaccination mandatory (Law 165/1991) for all newborns and for those who were 12 years old at the time.
Coinciding with World Hepatitis Day, “The Lancet Commission on Addressing the Global Hepatocellular Carcinoma Burden: Comprehensive Strategies from Prevention to Treatment” was published². It is a programmatic document that offers a detailed overview of the current state of art on hepatocellular carcinoma (HCC), discussing risk factors, etiology, and including reflections on challenges, effective strategies, and future perspectives. Liver cancer is the sixth most common and the third leading cause of cancer-related death worldwide. The number of new cases is expected to nearly double, from 870,000 in 2022 to 1,520,000 in 2050, if current trends are not reversed. The commission estimates that 60% of these cases are preventable by addressing modifiable risk factors such as hepatitis (through vaccination and medications), metabolic dysfunction-associated steatotic liver disease (MASLD), and alcohol consumption.
Hepatocellular carcinoma, the most common histological subtype, accounts for about 80% of all primary liver cancers. In Italy, in 2024, an estimated 12,610 new cases of HCC were diagnosed, with 33,800 people living after receiving a diagnosis³. Its incidence is linked to chronic liver diseases, such as viral hepatitis, alcohol-induced liver damage, and fatty liver disease.
Among the authors of the document – around fifty experts from Asia, the United States, and Europe – is Lorenza Rimassa, Associate Professor of Medical Oncology at Humanitas University and Head of the Hepatobiliopancreatic Tumors Section at Humanitas Research Hospital. She is the only Italian expert involved, contributing to the section on systemic therapies, i.e., oncological treatments. The paper proposes a comprehensive global approach covering the full course of the disease: from primary prevention to advanced care.
“This is not just a data summary, but a guiding document: a critical and constructive analysis of what works, what can be improved, and what actions can change the disease’s course,” explains Lorenza Rimassa. “The goal is to provide concrete recommendations, adaptable to local contexts, to reduce incidence and improve survival for patients worldwide.”
Among the contributions, the Italian Hepatitis C Screening Program was selected as a model example of prevention policy. It tackles the issue “upstream”: identifying and promptly treating the infection significantly reduces the long-term risk of developing liver cancer. In fact, 90% of cases arise from pre-existing chronic liver disease. The most common causes are: hepatitis B, hepatitis C, alcohol consumption, and – increasingly – MASLD, which is closely linked to obesity, hypertension, and dyslipidemia. A silent and increasing epidemic, not only in Western countries.
The availability of drugs and vaccines has led the WHO to define a global strategy to eliminate hepatitis. The ambitious goal, set by 2030, is to reduce new hepatitis B and C cases by 90% and reduce related mortality by 65%. For hepatitis B, this target is achievable thanks to vaccination for all newborns. For hepatitis C, elimination can be achieved by screening to detect positive individuals and providing immediate treatment.
“Hepatitis C screening has been available free of charge since 2020, on a voluntary basis, for those born between 1969 and 1989. It also includes the prison population and individuals followed by addiction services,” explains Alessio Aghemo, Full Professor of Gastroenterology and Director of the Department of Biomedical Sciences at Humanitas University and Head of the Internal Medicine and Hepatology Unit at Humanitas Research Hospital.
“So far, about 2 million people have been screened, with nearly 15,000 testing positive and 9,000 treated with direct-acting antiviral drugs. Italy has made great strides: it is now first in Europe for treated patients and seventh globally⁴. A result to be proud of, and a motivation to continue this path.”
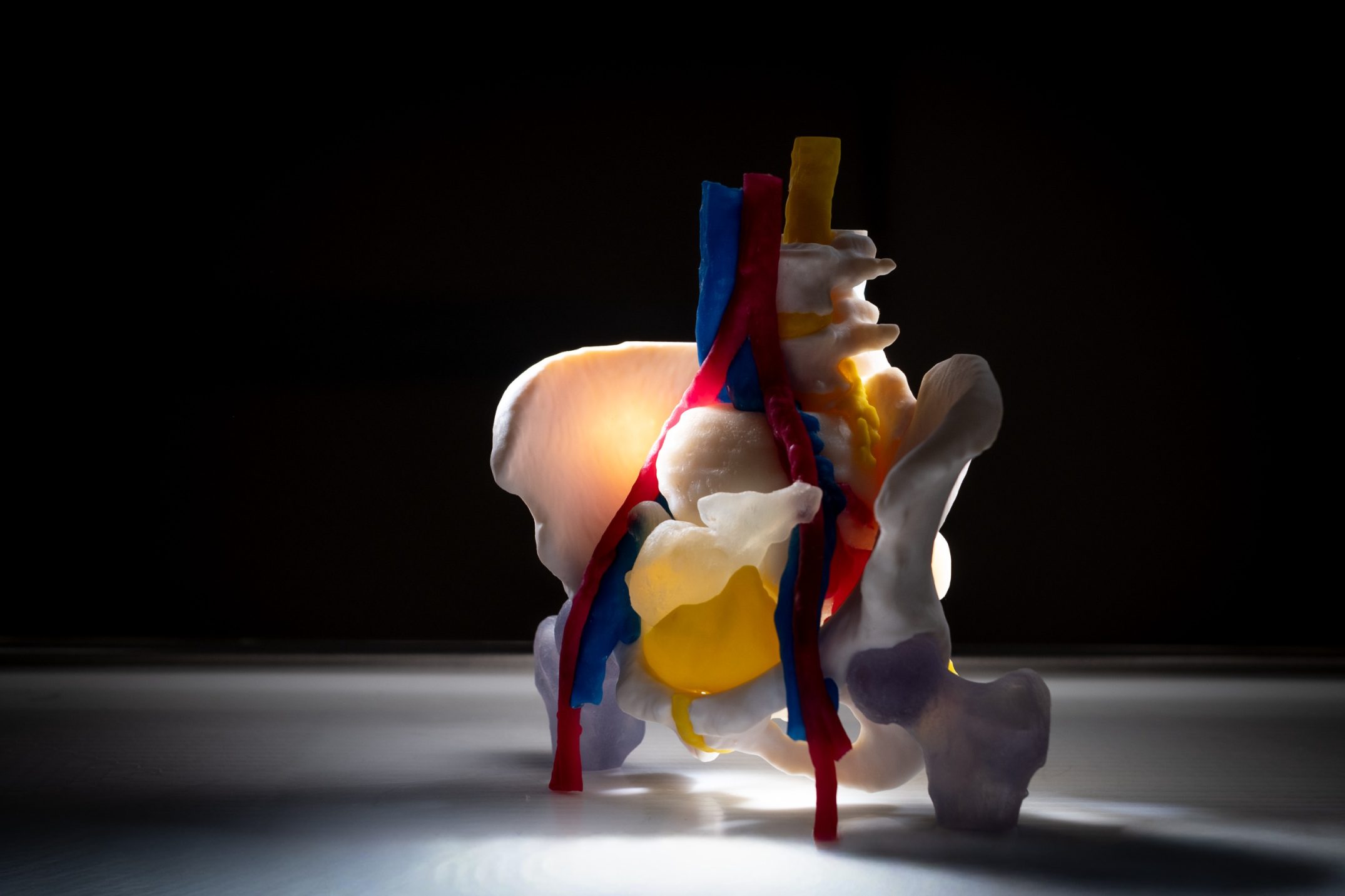
Today, there are several treatment options for hepatocellular carcinoma. “Treatment for HCC involves various therapeutic approaches and techniques, which can be used individually, in combination, or in sequence, depending on the stage of the tumor and the condition of the underlying liver disease,” explains Ana Lleo De Nalda, Full Professor at Humanitas University and Head of the Liver Immunopathology Laboratory at Humanitas. “From a surgical standpoint, we have valuable options for early-stage disease, including liver transplantation (in cases of decompensated cirrhosis or when the tumor fits within the so called ‘Milan criteria’) and surgical resection (when liver function is preserved). Both are considered radical treatments and can lead to a cure in a good percentage of cases.” Ablation, also a radical but non-surgical treatment, is used for single lesions up to 3 cm. Radiotherapy is available in various forms (e.g., radioembolization or stereotactic radiotherapy). When the disease is more advanced but still localized to the liver, the preferred option is intra-arterial therapies such as transarterial chemoembolization (TACE), a minimally invasive procedure that can be repeated as needed. “The goal of TACE is to control the disease over the long term – explains the expert – and allow good quality of life, although it does not lead to a cure. For this reason, studies are underway and have already shown promising results when combining immunotherapy with locoregional therapy, but we must wait for final data.”
In recent years, there have also been significant advances in treatment for advanced-stage hepatocellular carcinoma, which cannot be addressed with locoregional options. Several pharmacological therapies are now available. “For advanced HCC – says Rimassa – immunotherapy has revolutionized the therapeutic landscape. Currently, three combinations are approved by the FDA and EMA: atezolizumab + bevacizumab and durvalumab + tremelimumab (STRIDE regimen), both already reimbursed in Italy, and nivolumab + ipilimumab, still awaiting AIFA reimbursement. Compared to tyrosine kinase inhibitors, previously used as the first-line treatment and now used after immunotherapy, immunotherapy combinations offer longer survival and better quality of life, with fewer adverse events. In some cases, significant responses allow for reconsidering locoregional treatments, such as surgery.” A particularly noteworthy result comes from the STRIDE regimen, showing 5-year survival in 20% of patients⁵: an unprecedented figure for this disease.
References
- AISF Libro bianco – Le malattie epatiche definizione e ambiti e interventi per un approccio integrato – LS Cube 2024
- The Lancet Commission on Addressing the Global Hepatocellular Carcinoma Burden: Comprehensive Strategies from Prevention to Treatment. The Lancet. July 28, 2025: S0140-6736(25)01042-6. doi:10.1016/S0140-6736(25)01042-6.
- AIOM-AIRTUM-Fondazione AIOM-PASSI ISS 2024
- Razavi H et al., J Hepatol, in press
- Rimassa L, et al. Five-year overall survival update from the HIMALAYA study of tremelimumab plus durvalumab in unresectable HCC. J Hepatol. 2025 Apr 11: S0168-8278(25)00226-0. doi: 10.1016/j.jhep.2025.03.033. Epub ahead of print. PMID: 40222621